Dental Implant Surgery: Preparation, Procedure, and Patient Experiences
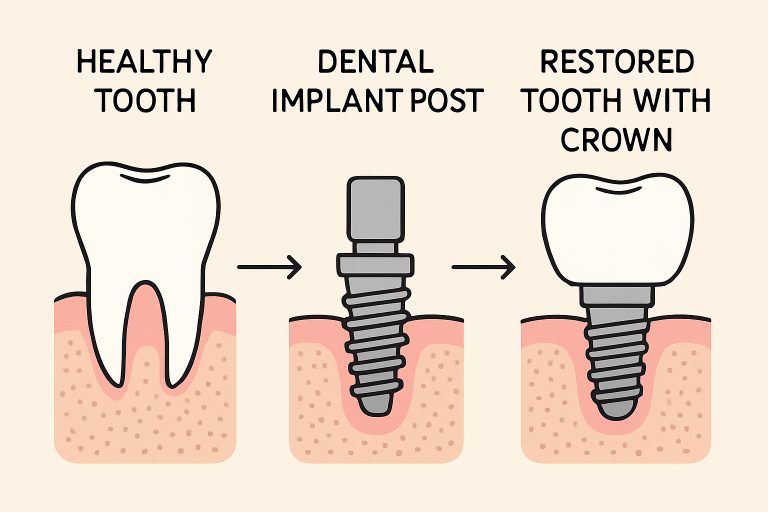
Table of Contents
- Preparation for Dental Implant Surgery
- The Dental Implant Procedure
- Patient Experiences and Outcomes
- Advancements in Dental Implant Technology
- Risks and Considerations
- Conclusion
Dental implants have rapidly transformed the landscape of restorative dentistry, providing patients with a strong, permanent option for replacing missing teeth. With technological advances and skilled practitioners, individuals seeking this treatment can anticipate functional and cosmetic benefits that far surpass those of traditional dentures or bridges. Those considering dental implants often begin by seeking expert care from institutions such as the Pikos Institute, known for pioneering techniques and quality patient care in implant dentistry.
Understanding every step of the dental implant journey—from initial preparation to the long-term patient experience—empowers individuals to make informed choices and feel greater confidence in their treatment options. Thorough preparation and professional guidance play vital roles in achieving optimal surgical outcomes while minimizing risks associated with the procedure. Dental implants not only restore smiles but can also dramatically improve overall oral health and quality of life.
Today, the dental field continues to evolve with innovations designed to make implant surgery safer, faster, and more predictable. Alongside these benefits, it’s also essential to recognize the potential challenges and considerations, including risks, candidacy, and aftercare. By gathering up-to-date information from reputable sources and specialists, patients can maximize the success and longevity of their implants.
For an in-depth understanding and support at every stage, working closely with both surgical experts and restorative dentists is crucial. Careful research and consultation ensure that each step—preparation, the procedure itself, and aftercare—aligns with the patient’s health history and personal needs.
Preparation for Dental Implant Surgery
Preparation is a critical phase that influences the success and longevity of a dental implant. The process starts with a comprehensive evaluation by your dentist or oral surgeon. This examination may include digital X-rays and advanced 3D dental imaging, which allow for detailed visualization of the jawbone’s shape and density. Accurate diagnostics not only help establish whether a patient has enough bone to support the implant but also reduce surgical risks.
- Comprehensive Dental Examination: An in-depth clinical and radiographic assessment is performed to evaluate existing teeth, gum health, and available bone structure.
- Review of Medical History: Disclosing all current and past medical conditions, medications, and lifestyle factors—such as smoking—ensures heightened safety. Certain underlying health issues may require special pre-surgical planning or antibiotic coverage.
- Custom Treatment Planning: Every implant case is unique. Some patients may need additional procedures, like bone grafting or sinus lifts, to optimize the bone foundation before implantation. Dental professionals develop a timeline and plan that addresses individual needs and goals.
The Dental Implant Procedure
The actual procedure unfolds over multiple stages and can span several months to allow for adequate healing and integration. According to Verywell Health, after the initial surgical placement of the implant, the site requires time for the bone to fuse with the implant before the replacement tooth can be attached. While every case has its nuances, most follow these key steps:
- Tooth Extraction: Damaged, decayed, or otherwise failing teeth are gently removed if they haven’t already been lost.
- Bone Grafting (if needed): Patients with insufficient jawbone density may require grafting procedures to establish a strong foundation for the implant.
- Implant Placement: A precision-crafted titanium post is surgically inserted into the jawbone. This minimally invasive step serves as the artificial root for the new tooth.
- Osseointegration: Healing takes place over weeks to several months. During this time, bone naturally fuses around the implant, anchoring it firmly in place for lifelong stability.
- Abutment Placement: After successful integration, an abutment—a small connecting piece—is attached to the implant post.
- Crown Placement: A custom-fabricated crown, designed to match the color and shape of the natural teeth, is placed onto the abutment, fully restoring the patient’s smile.
Patient Experiences and Outcomes
Patients widely report improved confidence, masticatory function, and overall health after successful implant surgery. While a degree of soreness, swelling, or minor discomfort is common in the days following each stage, complications are generally minimal with attentive postoperative care.
Several studies indicate high satisfaction rates among implant recipients, citing the normalized speech, improved oral hygiene, and ease of eating that dental implants enable. Many patients feel that their dental implants are indistinguishable from their natural teeth after the adjustment period.
Advancements in Dental Implant Technology
Modern dental implantology has benefited immensely from technological advances, shortening treatment times and optimizing outcomes. Innovations include:
- Guided Surgery: 3D cone-beam imaging and computer-guided design help create surgical guides, increasing precision and minimizing surgical trauma. This allows for more predictable outcomes and faster recovery times.
- Immediate Load Implants: When conditions are optimal, dentists can place a temporary crown on the same day as the implant surgery, streamlining the process and restoring function more rapidly.
Breakthroughs in materials and digital workflow are now enabling better integration, improved esthetics, and longer-life restorations.
Risks and Considerations
As with any surgical procedure, dental implant surgery has inherent risks. Recognizing and mitigating these risks is essential to maintaining oral health and implant longevity:
- Infection: Implants can occasionally develop peri-implantitis, a gum infection that can threaten the implant’s stability. Excellent oral hygiene and regular follow-up visits are crucial for prevention.
- Implant Failure: If proper bone integration does not occur, or if the site is exposed to undue stress (such as bruxism or smoking), the implant may fail and require removal or replacement.
- Nerve or Tissue Damage: In rare cases, surgery may injure surrounding structures, leading to numbness, tingling, or pain.
It is critical to work with experienced professionals who can assess medical suitability, utilize advanced diagnostics, and provide tailored aftercare to minimize these risks.
Conclusion
Dental implants represent the gold standard in modern tooth replacement, combining aesthetics, durability, and functionality. With thorough preparation, state-of-the-art procedures, and a commitment to aftercare, patients can reap long-term benefits and restored confidence. Staying informed and selecting expert care are key to a successful and satisfying dental implant journey.
